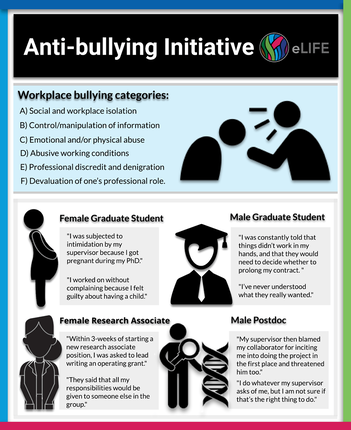
 Originally published on ecrLife (11/04/2019) https://ecrlife.org/bullying-in-academia-tales-from victims-and-a-call-to-action/ Nafisa M. Jadavji, Emily Furlong, Pawel Grzechnik, Małgorzata Anna Gazda, Sarah Hainer, Juniper Kiss, Renuka Kudva, Samantha Seah, Huanan Shi Workplace bullying--repetitive abusive, threatening, humiliating and intimidating behaviour--is on the rise globally. And matters are worse in academia. In the UK, for example, up to 42% of academics report being bullied in the workplace. The national average by contrast ranges from just 10-20%. Why do bullies bully? According to researchers from Brock University in Canada the goals of bullying come from internal motivations and desires, which can be conscious or not. Bullying takes many forms: the malicious mistreatment of someone including persistent criticism, inaccurate accusations, exclusion and ostracism, public humiliation, the spreading of rumors, setting people up to fail, or overloading someone with work. Bullying is different from accidental or reactive aggression, since it is goal-directed meaning that the purpose is to harm someone when there is a power imbalance. While anyone is at risk of being bullied in academia, research has found that some of us are more vulnerable compared to others. For example, early career researchers (ECRs), including trainees (e.g. graduate students, postdocs), minority groups, adjunct professors, research associates, and untenured professors are at a higher risk to experience bullying. Employees with more years in a job report feeling less bullied than others subordinate to them, meaning that junior members of a research group or Faculty may be at greater risk of bullying. An explanation for why particular groups are more vulnerable to bullying than others lies in the fact that the existence of power differentials are a major contributing factor to bullying in academia. For example, men and supervisors of large successful research groups are observed to perpetrate bullying behavior more often than women and other minorities, though exceptions do exist. Other research has shown that the pressure associated with publishing, getting research funding, and lack of leadership and people management training in science may also contribute to bullying. In some cases, principal investigators (PI) can also experience bullying from students, peers, or administrators. Take the example of one PI who was bullied by an administrator for being too ambitious, making her overly conscious of her success. When she moved to another institution, she did not make collaborations with other researchers in different departments, as she had previously, because she did not want to appear to be too ambitious. This is also an example of the long-term impact bullying can have on future work. To highlight that bullying can take different forms and occur at all career stages, we include here four anonymous testimonials from victims of academic bullying in the life sciences: International Female PhD Student I got pregnant during my PhD and I was told it was not an issue. However, during the course of my pregnancy, I was removed from my projects and left out of discussions about the work that needed to be done. When I asked for an explanation, I was told that science could not wait for me while I was pregnant, even though I was eager to work, and the law permitted me to do so. After my child was born, I was made to return to work after just three weeks, while legally I was permitted up to a year off work. In the lab, I was given bits and pieces of others’ projects and not permitted to work on my own project. I worked without complaining but this took a toll on my emotional health with time. It was after my then-toddler son broke his arm that everything got worse. I needed to take a week off for his hospital stay, but my supervisor called me to his office and told me that I was a useless researcher and that I didn’t belong in science, and then he fired me. I knew it was illegal for him to do so, but I didn’t want to fight him because I was dependent on him to finish my PhD. I met with him after a week and he told me that I could work, but without pay, to make up for the duration of my pregnancy when I was paid. I did as I was told for the next six months, and somehow with the support of my husband and my best friend, was able to graduate and leave. I now have a permanent faculty position at a university in my home country, but my PhD broke me. Male Graduate Student Completing His Graduate Studies in His Home Country After I joined the lab, my supervisors told me that they needed to re-apply for funding, and that they were relying on my results for the application. Unfortunately, they wanted to employ a method that they were unfamiliar with, and as a beginner, I had very limited resources. I managed to get help from someone at another department and it took me three months to set up the method in the lab, but it turned out to be unsuitable for our project. My supervisors were unhappy about this and started blaming me for not smart enough to get the results they expected. I was constantly told that things didn’t work in my hands, and that they would need to decide whether to prolong my contract. This threat was dangled in front of me every few months, and it scared me. I contemplated leaving the lab and moving on, but my supervisors told me that it would look bad for them and offered me another project instead. Things didn’t improve after this either: my project worked fine, but my supervisors continued threatening to terminate my contract. I decided to graduate after three and a half years of enduring this, but my supervisors then threatened to block me from finishing. I was gas lighted throughout my Master’s and never understood what they really wanted. Why did they offer me a position if I wasn’t good enough? I decided to switch fields after my PhD and am much happier now. Female Research Associate in Home Country Within 3-weeks of starting a new research associate position, I was asked to lead the writing of a grant. The research focus of the group was beyond my experience, and I had little exposure to the research environment of the group. The PI had not established the big picture of the grant; it was left up to me. Furthermore, he provided little to no guidance with writing the grant (e.g. his expectations, what had previously been done, etc.). It was a very overwhelming experience. When I sent out a draft of the grant, I was pulled into a private meeting with the PI and the co-PI, who both told me that my work was crap and that since I was the highest paid member of the group I should have been producing amazing work. They said that all my responsibilities would be given to someone else in the group. I was given menial tasks like uploading files on the One Drive for several months. Most days, I would not have enough work to do or struggle with the work I was required to do because there was not enough guidance. I have been doing research for 16 years but had never been so bored as I was in this position. A few months later, I was asked to do a few more projects, but again was told my work was not good. The culture in the research group was unforgiving and exclusive. Outside of the job, through my hard work and determination, I obtained another position and was able to leave. When I sent in my resignation, I was even intimidated to leave earlier than I planned because it would cost them less. I stood my ground and left when I planned to. This job increased my imposter syndrome by a hundred-fold. I was convinced that I was the problem and the dumb one. When I told my husband about the interactions with the PI, he would comment on how ridiculous the situation was. When I was in this situation, it was too hard to see how crappy it was. It’s been about a month since I left, and I feel so much better. I have worked hard to combat my imposter syndrome, and this summer I will begin a tenure track position in a STEM field. In 2019, this is so rare, so I celebrate that! International Male Postdoc I work as a postdoctoral researcher and my supervisor routinely tells us whom we can talk to, eat our lunch or take coffee breaks with. I recently started collaborating on a project with another postdoctoral researcher in the department but only after discussing it with my supervisor and gaining his approval. We worked on the project part-time for a few months. I approached my supervisor after we had some interesting results, and he suddenly decided that I needed to stop working on it despite the fact that it looked promising. He informed me that he was shocked that I was working on it in the first place and that he didn’t like me to do things behind his back. He also accused me of leaving him out of my activities in the lab. I was also tasked with informing my collaborator, who was livid that we needed to end the project abruptly. However, he understood and let it go, even though it was unfair for him too. My supervisor then blamed my collaborator for inciting me into doing the project in the first place and threatened him too. I do whatever my supervisor asks of me, but I am not sure if that’s the right thing to do. Unfortunately, I feel as though I have no choice since he pays me. The impacts of bullying are manifold. Studies have reported a long-term health effects in bullying victims, such as anxiety, sleep disorders, chronic fatigue, anger, depression, destabilization of identity, aggression, low self-esteem, loss of confidence, and other health problems. Bullying also has an impact on the institutions where the victims work, including negative work environments, absenteeism, lower engagement, higher turnover, and reduced performance. The impact of bullying is far reaching, policies need to be put into place to tackle the negative impact. Recognizing what bullying looks like is just the first step towards tackling it. Many institutions have opted to use a top-down approach to tackle the problem through policies to report bullying via the human resource office or sometimes an ombudsman. Other institutions may not have specific policies to deal with bullying and often victims are not made aware of existing avenues of recourse. Funding agencies may also choose to get involved, for example after being accused of bullying by her colleagues in 2018 Professor Nazneem Rahman lost 3.5 million GBP in funding from the Wellcome Trust in the UK. In addition to what is currently being done at research institutions and funding agencies, legislation should be put into place by the government to ensure that victims are heard and that there are consequences for the perpetrators. Apart from institutional actions, bottom-up approaches are also available, such as overcoming the bystander effect. The bystander effect is when individuals are less likely to offer help to a victim when other people are present. Research since the 60s has shown that the presence of other people will inhibit one’s own intention to help and overcoming this effect could be an effective way to mitigate bullying in academia. A study of whistleblowers found that 71% of employees tend not to directly report wrongdoing as the perceived personal cost is higher than the perceived reward. People tend to feel that personal costs may be higher if reporting happens through face-to-face meetings with authorities. Hence, anonymous reporting channels are needed. Bullying is an entrenched problem in academia, supported by workplaces with power differentials. Combating bullying is a challenging task at multiple levels and over the next year a group of us eLife Community Ambassadors will embark on an initiative to shine a light on the problem, investigate its root causes and eventually formulate a set of universal measures to tackle bullying in the workplace and give relief to its victims. Stay tuned for more on our progress!
2 Comments
I wrote this blog post for the American Society for Nutrition.
Parkinson’s disease (PD) is a neurodegenerative disease, this means that the damage in the brain begins several decades before the symptoms appear. In PD, approximately 60% of a specific cell type in the brain die before symptoms appear. The cells that die are dopamine producing cells. Dopamine is a neurotransmitter, which is a chemical in the brain that help cells communicate with each other. Dopamine cells within the substantia nigra, an area of the brain, die in PD. In the figure above you can see dopamine producing cells. PD was first described in 1817 by James Parkinson and the exact cause of PD still remains unknown, researchers and clinicians know that changes in our DNA plays an important role. There is also an environmental component, for example exposure herbicides like paraquat induce PD in people. Another example of an environmental contributor is nutrition. Nutrition, specifically B-vitamins, have been implicated in the onset and progression of PD. An example of a B-vitamin is folic acid, which is well known for its’ role in preventing neural tube defects during early brain development. Additionally, folic acid also helps lower levels of a chemical called homocysteine. High levels of homocysteine are present in PD patients that take levodopa (L-DOPA), a pharmaceutical drug that helps replenish dopamine in the brain. The breakdown of L-DOPA in the body requires methyl groups generated from folic acid, this in turn increases levels of homocysteine. A protein that breaks down folic acid to generate methyl groups is called methylenetetrahydrofolate reductase (MTHFR) and people with reduced levels of this protein are reported to be more affected by PD. In a recent research study from our group we use a mouse model with reduced levels of MTHFR to study how the paraquat model of PD impacts onset and progression. Our study found that reduced levels of MTHFR result in motor impairments in PD mice, these impairments are characteristic of PD. Additionally, the PD mice were sick and had higher had higher levels of inflammation in the substantia nigra. There were also high levels of oxidative stress, which is an imbalance of reactive oxygen and antioxidant production within a brain region closely connected to the substantia nigra. Higher levels of oxidative stress have been implicated in several neurodegenerative diseases. In terms of targeting oxidative stress through pharmaceuticals there has not been much progress. Food stuffs such as red wine, green tea, and blueberries have been reported reduce levels of oxidative stress, through their antioxidant properties, but more investigation is required. Nutrition is an important aspect of health. It is well documented that not all older adults absorb as many nutrients compared to their younger counterparts due to several factors, one being inflammation in the stomach. These recent research findings presented in this blog along with others suggest that adequate nutrition should be a component of health care for patients with PD. I wrote this blog post for the American Society of Nutrition.
According to the United Nations the aging population is growing and by 2050 the number of people aged 60 years old will reach 2 billion worldwide. With the aging population the prevalence of age-related disease is predicted to increase. An example of an age-related disease is neurodegeneration. Dementia can be a result of several pathologies including increased levels of Lewy bodies, as seen in Parkinson’s disease. Cerebrovascular disease is the second most common cause of dementia and is a result of changes in blood flow to or within the brain. Blood flow in the brain can changes because of hypertension, diabetes, smoking, and hypercholesterolemia. Patients with cerebrovascular disease experience cognitive impairment, specifically when trying to remember things or plan events/trips. It is important to note that symptoms can vary from patient to patient. A type of cerebrovascular disease is vascular cognitive impairment. Nutrition is modifiable risk factor for diseases of aging. As people age their ability to absorb nutrients from their diet decreases. Several studies have reported that changes in B-vitamins may play a role in the onset and progression of dementia. Additionally, a study by researchers in the United Kingdom shown that B-vitamin supplementation reduced brain volume loss in areas associated with cognitive decline. A recent international consensus statement from leaders in the field suggests that deficiencies in B-vitamin metabolism should be considered when screening dementia patients. My research using model organisms has tried to understand the diseases processes associated with dementia. Using a mouse model of VCI we have reported that deficiencies in folic acid, either dietary or genetic affect the onset and progression of VCI. Using the Morris water maze task we report that mice with VCI and folate deficiency performed significantly worse compared to controls. We assessed changes in the brain using MRI and interestingly found that folate deficiency changed the vasculature in the brain of mice with VCI. Because of either a genetic or dietary folate deficiency all the mice had increased levels of homocysteine. Our results suggest that it is not elevated levels of homocysteine making the brain more vulnerable to damage, but the deficiency in folic acid, either dietary or genetic that changes the brain. In the cell folic acid is involved in DNA synthesis and repair as well as methylation. These are vital functions for normal cell function. Therefore, reduced levels of folate may be changing the cells in the brain and making them more vulnerable to any types of damage. We think that high levels of homocysteine may just be an indication of some deficiency (e.g. reduced dietary intake of folic acid). Maintaining normal levels of homocysteine are needed, since studies in humans have shown that elevated levels in homocysteine are a risk factor for neurodegenerative diseases and that reducing them is beneficial. Folic acid is a B-vitamin and is well known for its role during early neurodevelopment. It promotes the closure of the neural tube in utero. The neural tube in the developing embryo is the first step to forming the brain and spinal cord. If the neural tube does not close, it can lead to neural tube defects (NTDs), such as spina bifida. Women of child bearing age are recommended to supplement their diet with 0.4 -1 mg of folic acid daily. Additionally, to reduce the number of NTDs mandatory folic acid fortification laws were put into place in 1998 in the US and Canada, as well as other countries around the world. In response to mandatory fortification, there has been a reduction in the number of NTDs in both Canada and the US.
Recently, maternal over supplementation of folic acid has raised some concerns. Over supplementation is defined as ingesting over 1 mg of folic acid daily. There has been an increase in over supplementation of folic acid in the US and Canada where mandatory folic acid fortification laws are in place and supplement use is high. Epidemiological studies have reported that too much folic acid has been associated with increased risk of cancer. Interestingly, too much maternal folic acid intake has been associated with autism spectrum disorder, but the data is not clear as other studies have reported the protective effects. Furthermore, too much maternal folic acid has been reported to change neurodevelopment in animals. A recent published study investigated whether too much maternal folic acid is associated with changes in the neurodevelopment of offspring. Using a mouse model of maternal over supplementation of folic acid the authors report that male offspring from mothers that were fed high levels of folic acid had impaired memory and brain development. The amount of folic acid in the diet of mothers was 20mg/kg to model over supplementation in humans. Animals from mothers with over supplementation of folic acid did not remember seeing a familiar object as well as control animals did. Furthermore, they had reduced levels of a neurotransmitter that is important in learning and memory called acetylcholine. These are some of the first results showing how maternal over supplementation with folic acid may affect early neurodevelopment. We recently published an up-to-date review of how maternal over supplementation of folic acid impacts offspring neurodevelopment. Our comprehensive analysis includes studies from human populations as well as basic science studies to understand how things in the brain as well as behaviors are changing when mothers are supplementing with too much folic acid. More studies are required to understand the full impact of how maternal over supplementation studies affect offspring neurological development. As someone wise once said, everything in moderation. I wrote this post the Addictive Brain, originally posted here.
The brain is a very complex organ and requires a lot of resources from the body. I am a neuroscientist that studies the brain and how what we eat impacts brain function. The component of nutrition that my research focuses on is called folic acid, which is a B-vitamin. Folic acid is a water-soluble vitamin, meaning that it does not stay in our body for very long, so we need a constant intake. The bacteria in our gut makes a bit of folic acid, but not enough to meet our body’s requirements. The food that we eat is a good source of folic acid. Food like leafy greens, lentils, and liver are all a good source of folic acid. Most people know folic acid because of its’ protective role during early brain development. Women that are of child bearing age are recommended to take folic acid prior to getting pregnant because the vitamin helps close the neural tube. The neural tube is future brain and spinal cord. If the neural tube does not close, it can lead to the development of neural tube defects (NTDs) in babies, such as spina bifida. To prevent the NTDs, mandatory folic acid fortification laws were put into place in 1998 in both the US and Canada, as well as other countries. It is important to note that since 1998 there has been a reduction in the number of NTDs in both Canada and the US. To understand how folic acid impacts brain function, my research uses mice. I am going to share with you 2 studies that have examined the role of maternal dietary folic acid intake on offspring brain and behavior function. In the first study, female mice were put on a folic acid deficient diet prior to pregnancy and remained on the same diet after they gave birth. When the pups were 3-weeks-of-age, I tested their memory function. Three-week-old mice are equivalent to young adults. I found that pups were on a folic acid deficient diet had impaired memory compared to control diet. These mice also had changes in the area of the brain called the hippocampus, which is well known for its’ role in learning and memory. In hippocampi of folic acid deficient diet pups, I found reduced levels of acetylcholine, a neurotransmitter. These findings suggest that maternal folic acid impairs brain function after birth. These data suggest that folic acid is may not only needed prior to pregnancy, but also during pregnancy. Last year, we published a study investigating whether too much maternal folic acid is associated with changes in the neurodevelopment of offspring. Using a mouse model of maternal over supplementation of folic acid we report that male offspring from mothers that were fed high levels of folic acid had impaired memory and brain development. These are some of the first results showing how maternal over supplementation with folic acid may affect early neurodevelopment. More studies are required to further dissect the mechanisms as well as determine if the benefits continue into adulthood. As someone wise once said, everything in moderation. This blog post was published on the American Society for Nutrition, in May 2018.
A stroke occurs when there is reduced blood flow to the brain. Blood carries oxygen and glucose to cells in the brain. When there is reduced levels of blood, these cells start to die. Since the brain controls behavior, this cell death leads to impairments in function. The impairments are dependent on where the stroke happens in the brain. There are two main types of stroke, hemorrhagic and ischemic. For this blog, I will be focusing on ischemic stroke which is a result of blockage in a blood vessel. Currently, stroke affects older individuals and the global population is aging according to the United Nations. Additionally, older individuals also lose their ability to absorb all the vitamins and nutrients they require from their diet as they age. Nutrition is a modifiable risk factor for diseases of aging. For example, B-vitamins absorption decreases as individuals age. B-vitamins play a major role in reducing levels of homocysteine, a non-protein amino acid. High levels of homocysteine have been associated with increased risk to develop cardiovascular diseases, such as stroke. Supplementation with B-vitamins has been reported to have positive effects on brain health. A study by researchers in Oxford University and University of Oslo has shown that B-vitamin supplementation in the elderly within the United Kingdom reduced age-related brain atrophy after 2 years of supplementation. Furthermore, another study by the same group reported that B-vitamin supplementation reduced cerebral atrophy in areas vulnerable to Alzheimer’s disease. More recently, a group from China reported that folic acid supplementation in combination with Enalapril, used to treat heard disease, reduced the risk of stroke by 21% in patients that were hypertensive. Within the aging population, B-vitamin supplementation has been reported to have positive effects on brain health. The elderly are more prone to ischemic stroke, but the mechanisms through which this benefit accomplished is not well understood. A recent study investigating the role of B-vitamin supplementation on ischemic stroke was published in the Neurobiology of disease. This study tried to examine the mechanisms of how supplementation improved brain function. A group of wildtype males were put on a folic acid deficient diet (0.2 mg/kg) prior to ischemic damage to increase levels of homocysteine and another group of mice were put on a control diet (2mg/kg folic acid). After ischemic damage to the sensorimotor cortex, FADD mice were put on a supplemented diet, where levels of folic acid, riboflavin, vitamin B12, and choline were increased. Animals were maintained on the diets for 4-weeks after which motor function was assessed. Researchers found that supplemented diet mice performed better on motor tasks compared to CD mice with ischemic damage. In the brain tissue increased levels of plasticity and antioxidant activity were reported. Combination therapies for stroke affected patients are thought to be most effective. A pharmaceutical in combination with a life style change, such as increase exercise may be beneficial for stroke affected patients. This data suggests that nutrition may also be a viable option for life style change ischemic damage. Folic acid is a B-vitamin and is well known for its role during early neurodevelopment. It promotes the closure of the neural tube in utero. The neural tube in the developing embryo is the first step to forming the brain and spinal cord during in utero neurodevelopment. If the neural tube does not close, it leads to neural tube defects (NTDs) in babies, such as spina bifida (Lemire, 1988). Women of child bearing age are recommended to take 0.4 -1 mg of folic acid supplements daily. Additionally, to reduce the number of NTDs mandatory folic acid fortification laws were put into place in 1998 in the US and Canada, as well as other countries. Since 1998, there has been a reduction in the number of NTDs in both Canada and the US (Castillo-Lancellotti et al., 2013).
The brain begins developing a few days after implantation and continues until the individual is in his or her mid-twenties. During neurodevelopment, the short-term impact of folic acid is well known, but the long-term effects are not well defined. This article will describe recent data that shows long term effects of maternal deficiency on offspring memory function. On the other side, maternal over supplementation of folic acid has recently been reported to have negative effects on neurodevelopment. Over supplementation is defined as ingesting over 1 mg of folic acid daily. Using a mouse model, we investigated the long-term effects of maternal deficiencies of folic acid on offspring memory function. Female mice were put on a diet deficient in folic acid prior to pregnancy (Jadavji et al., 2015). The impact of maternal deficiency on offspring memory function was evaluated. The offspring were ~3 weeks which is equivalent to young adults. Our research findings suggest that offspring from moms with a folic acid deficiency had impaired short-term visual memory. This may be a result of increased cell death and reduced cell proliferation within the hippocampus, a structure in the brain that is involved in memory. Being folic acid deficient is not recommended for women of child bearing age, not only to avoid NTD, but also for neurodevelopment after birth. Recently, there have been concerns about over supplementation of folic acid in countries like Canada where mandatory folic acid fortification laws are in place and supplement use is high (Patel and Sobczynska-Malefora, 2017). In epidemiological studies, too much folic acid has been associated with increased risk of cancer (Boyles et al., 2016). Interestingly, too much maternal folic acid intake has been associated with autism spectrum disorder (Beard et al., 2011), but the data is not clear as other studies have reported the protective effects (Wang et al., 2017). Furthermore, too much maternal folic acid has been reported to impair other neurodevelopmental aspects of the brain and behavior in offspring (Roth et al., 2011). We recently published a study (Bahous et al., 2017) investigating whether too much maternal folic acid is associated with changes in the neurodevelopment of offspring. Using a mouse model of maternal over supplementation of folic acid we report that male offspring from mothers that were fed high levels of folic acid had impaired memory and brain development. The amount of folic acid in the diet of mothers was 20mg/kg to model over supplementation in humans. Mothers were supplemented for 6 weeks prior to pregnancy and throughout lactation. Once we weaned the pups from mothers they were maintained on supplemented diet until we collected experimental data. We assessed short-term memory of mice using a test called the novel object recognition, animals from mothers with too much folic acid did not remember seeing a familiar object as well as control animals did. Furthermore, they had reduced levels of a neurotransmitter that is important in learning and memory called acetylcholine. The pups from mothers over supplemented folic acid mothers had altered development of the cortex. This means that part of their brain did not follow normal development patterns. Interestingly the offspring from maternally over supplemented folic acid mother showed a similar phenotype to that of mice with a genetic deficiency in folic acid metabolism (Jadavji et al., 2012). These are some of the first results showing how maternal over supplementation with folic acid may affect early neurodevelopment. More studies are required to further dissect the mechanisms as well as determine if the benefits continue into adulthood. As someone wise once said, everything in moderation. I wrote this post for the website called Women in Science in 2017.
I am a female Canadian Neuroscientist interested in how nutrition, specifically B-vitamins and age impact brain function. The B-vitamin I work closely with is called folic acid, it is well known for its role during early neurodevelopment. Specifically, for the closure of the neural tube in utero. The neural tube in embryos is the first step to forming the brain and spinal cord. If the neural tube does not close, it leads to the development of neural tube defects (NTDs) in babies, such as spina bifida. To prevent the NTDs, mandatory folic acid fortification laws were put into place in 1998 in the US and Canada, as well as other countries. Since 1998 there has been a reduction in the number of NTDs in both Canada and the US. Recently, there have been concerns about over supplementation of folic acid in countries like Canada where mandatory folic acid fortification laws are in place and supplement use is high (Patel and Sobczynska-Malefora, 2017). In epidemiological studies, too much folic acid has been associated with increased risk of cancer (Boyles et al., 2016). Interestingly, too much maternal folic acid intake has been associated with autism spectrum disorder (Beard et al., 2011), but the data is not clear as other studies have reported the protective effects (Wang et al., 2017). Furthermore, too much maternal folic acid has been reported to impair other neurodevelopmental aspects of the brain and behavior in offspring (Roth et al., 2011). We recently published a study (Bahous et al., 2017) investigating whether too much maternal folic acid is associated with changes in the neurodevelopment of offspring. Using a mouse model of maternal over supplementation of folic acid we report that male offspring from mothers that were fed high levels of folic acid had impaired memory and brain development. The amount of folic acid in the diet of mothers was minimal (5mg/kg of folic acid) and comparable to human supplementation. Mothers were supplemented for 6 weeks prior to pregnancy and throughout lactation. Once we weaned the pups from mothers they were maintained on supplemented diet until we collected experimental data. We assessed short-term memory of mice using a test called the novel object recognition, animals from mothers with too much folic acid did not remember seeing a familiar object as well as control animals did. Furthermore, they had reduced levels of a neurotransmitter that is important in learning and memory called acetylcholine. The pups from mothers over supplemented folic acid mothers had altered development of the cortex. Interestingly the offspring from maternally over supplemented folic acid mother showed a similar phenotype to that of mice with in born error of metabolism (Jadavji et al., 2012). These are some of the first results showing how maternal over supplementation with folic acid may affect early neurodevelopment. More studies are required to further dissect the mechanisms as well as determine if the benefits continue into adulthood. As someone wise once said, everything in moderation For Canada's 150th Birthday, my research was profiled in the Faces of Health Research, by the Canadian Institutes of Health Research (CIHR).
Dr. Nafisa M. Jadavji Carleton University Vascular cognitive impairment (VCI) is the second leading cause of dementia after Alzheimer's disease. The clinical presentation of VCI varies and there are no treatments for VCI since the actual pathology remains unknown. Nutrition is a risk factor for VCI, specifically high levels of homocysteine, a common amino acid in blood. B vitamins, such as folic acid, can reduce levels of homocysteine. My research program focuses on how nutrition affects the brain. Our results suggest that it is not elevated levels of homocysteine making the brain more vulnerable to VCI, but rather, a deficiency in folic acid. In the cell, folic acid is involved in essential functions that help the cell survival. Reduced levels of folic acid may be changing the cells in the brain, making them more vulnerable to damage. More research is required to understand how nutrition can be used to promote healthy brain aging. This blog post was written for AlzScience, in 2017. It describes in lay term my
High levels of homocysteine have been implicated in neurodegenerative diseases, such as dementia, mild cognitive impairment, and Alzheimer’s disease. Homocysteine can be measured in blood easily, which has led to several studies in humans reporting that elevated levels of homocysteine lead to increased risk of developing neurodegenerative diseases or affect progression. Interestingly, homocysteine levels in our bodies increase as we age. Vascular cognitive impairment (VCI) is the second leading cause of dementia after Alzheimer’s disease. VCI is the result of reduced blood flow to the brain, however, the pathology is not well understood. Reduced blood flow ben be a result of age and health (e.g. high cholesterol). The clinical presentation of VCI varies, most the patients have some degree of cognitive decline. There are currently no treatments for VCI since the actual pathology remains unknown. Nutrition is a risk factor for VCI, specifically high levels of homocysteine. High levels of homocysteine can be reduced by B-vitamins, like folates or folic acid. Folates are the natural occurring form of the vitamin, these are often found in food such as green leafy vegetables or liver. Whereas folic acid is the chemically synthesized form that is often taken in supplemental form. My research program focuses on how nutrition affects the brain, specifically how folates affect neurodegeneration. Using a mouse model of VCI we have reported that deficiencies in folates, either dietary or genetic, affect the onset and progression of VCI. Using the Morris water maze task, we report that mice with VCI and folate deficiency performed significantly worse compared to controls. We assessed changes in the brain using MRI and interestingly found that folate deficiency changed the vasculature in the brain of mice with VCI. Because of either a genetic or dietary folate deficiency, all the mice had increased levels of homocysteine. However, we did not observe any significant association between elevated levels of homocysteine and behavioral impairment or changes in the brain tissue of VCI affected mice. Our results suggest that it is not elevated levels of homocysteine making the brain more vulnerable to damage, but the deficiency in folates, either dietary or genetic that changes the brain. In the cell, folates are involved in DNA synthesis and repair as well as methylation. These are vital functions for normal cell function. Therefore, reduced levels of folate may be changing the cells in the brain and making them more vulnerable to any types of damage. I would like to suggest that high levels of homocysteine may just be out put measurement of some sort of deficiency (e.g. reduced dietary intake of folates). Several studies using brain cells that are grown in petri dishes have reported that extremely high levels of homocysteine need to be added to cells to cause damage. These levels are usually not observed in humans. In terms of future directions, more research is required to understand how deficiencies in folates, homocysteine and other nutrients that reduce levels of homocysteine like choline change cells in the brain throughout life and how these changes are related to neurodegeneration. |
Archives
December 2023
Categories |

 RSS Feed
RSS Feed